As we transition into a new era in health care post the COVID-19 pandemic, the evolving landscape of telehealth regulations can be challenging to navigate. The California Telehealth Resource Center (CTRC) acknowledges this complexity and aims to shed light on the recent shifts in telehealth regulatory requirements. As a trusted, free, and unbiased resource for both providers and patients, we are dedicated to offering clear, up-to-date telehealth information to help you understand these significant changes.
During the pandemic, telehealth surged in prominence, becoming an essential healthcare delivery modality. Now, with the federal COVID-19 Public Health Emergency (PHE) declaration having ended on May 11, 2023, it’s important for providers and patients alike to stay informed of the termination of some COVID-19 PHE telehealth flexibilities, temporary extensions, and, in some cases, permanent extensions. In this post, we highlight the recent Medicare payment policy changes, what’s been extended, and what’s now permanently etched into the landscape of telehealth.
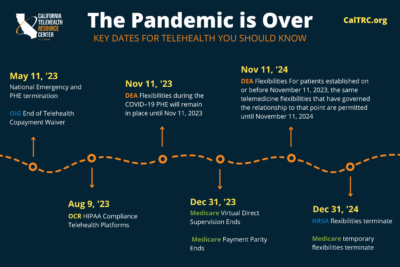
It is important to note that there are various rules from the DEA, the OIG, HRSA, and other government entities that differ from the information below. If you have specific questions, please reach out to our team at CalTRC@ochin.org or utilize CTRC’s updated PHE timeline to view key dates in telehealth (pictured below).
 Regulatory Medicare Changes Affecting Telehealth
Regulatory Medicare Changes Affecting Telehealth
With the end of the COVID-19 Public Health Emergency (PHE), the Medicare landscape for telehealth services has experienced significant alterations. It is important to understand that these changes are of two types: those that have become permanent fixtures in the provision of telehealth services and those that have been given a temporary extension through the end of 2024.
The permanent changes, enacted through several regulatory changes and policies, reflect the growing recognition of the importance and efficacy of telehealth. For instance, Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) have been granted the authority to serve as distant site providers for behavioral/mental telehealth services, with patients now able to receive these services in their homes, regardless of geographic restrictions. Additionally, behavioral/mental telehealth services can now be delivered using audio-only communication platforms.
In the same vein, Rural Emergency Hospitals (REHs) have been made eligible as originating sites for telehealth. These changes mark a significant step forward in enhancing access to behavioral and mental health services through telehealth, particularly in rural and underserved areas.
On the other hand, temporary extensions have been granted for certain telehealth flexibilities until December 31, 2024. For instance, FQHCs and RHCs can now serve as distant site providers for non-behavioral/mental telehealth services. Medicare patients can receive these telehealth services in their homes, again, without geographic restrictions.
Moreover, some non-behavioral/mental health services can be delivered using audio-only platforms, and the requirement for an in-person visit within six months of an initial behavioral/mental telehealth service and annually thereafter is currently not required. Telehealth services can also be provided by all eligible Medicare providers during this period. Eligible specialty types for Medicare include:
Physicians
- Doctors of medicine or osteopathy
- Doctors of dental medicine
- Doctors of dental surgery
- Doctors of podiatric medicine
- Doctors of optometry (Optometrists can only order DMEPOS supplies and laboratory or x-ray services payable under Medicare Part B.)
Non-Physician Practitioners
- Physician Assistants
- Clinical Nurse Specialists
- Nurse Practitioners
- Clinical Psychologists
- Interns, Residents, and Fellows
- Certified Nurse Midwives
- Clinical Social Workers
If you have any questions regarding your eligibility, please contact your Medicare Administrative Contractor (MAC).
Understanding these permanent and temporary changes is crucial for health care providers as they plan their telehealth strategy in the coming years and for patients seeking to understand how their access to telehealth services may evolve. These aforementioned changes are listed below for clarity.
Permanent Medicare Changes
The permanent changes primarily pertain to the provision of behavioral and mental health services, as authorized by the Consolidated Appropriations Acts of 2021 and 2022 and the CMS CY 2022 and 2023 Physician Fee Schedules. Key changes include:
- Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) can provide behavioral/mental telehealth services
- Medicare patients can receive behavioral/mental telehealth services at home
- There are no geographic restrictions for originating sites for behavioral/mental telehealth
- Behavioral/mental telehealth services can be delivered using audio-only communication platforms
- Rural Emergency Hospitals (REHs) meet the criteria to serve as originating sites for telehealth
Temporary Medicare Changes (Through December 31, 2024)
Some temporary changes under the Consolidated Appropriations Act of 2023 also apply. These include:
- FQHCs and RHCs can provide non-behavioral/mental telehealth services
- Medicare patients can receive telehealth services at home
- There are no geographic restrictions for originating sites for non-behavioral/mental telehealth services
- Some non-behavioral/mental telehealth services can be delivered using audio-only communication platforms
- An in-person visit within six months of an initial behavioral/mental telehealth service and annually thereafter is not required
- Telehealth services can be provided by all eligible Medicare providers
The Future of Telehealth
While the extension of these telehealth flexibilities through the end of 2024 is a positive step, there is still much to be determined about the long-term status of telehealth in the post-pandemic era. As with any significant healthcare reform, continued monitoring and advocacy are crucial.
With the commitment of healthcare providers, policymakers, and advocates, the hope is that the healthcare community can continue to leverage the power of telehealth to improve access to care for all patients, regardless of their location or circumstances.
For further updates and in-depth resources on telehealth, don’t hesitate to reach out to our team of unbiased experts at CalTRC@ochin.org or explore the wealth of materials available on our website.


Leave a Comment