Lesson 4 of 6
Medi-Cal
FFS Medi-Cal Billing Requirements for Virtual/Telephonic Communications
On February 3rd, 2022, DHCS updated their Medi-Cal Billing requirements for Virtual/Telephonic Communications.
FQHCs/RHCs are able to bill their PPS rate, as applicable, for live video telehealth and telephone services.
Patients do NOT have to be HHMS to be seen in their home during the public health emergency.
Medi-Cal also released a COVID-19 PHE Operational Unwinding Plan on August 22, 2022. This includes information on Medi-Cals global unwinding approach in regards to Telehealth and Medi-Cal, Medi-Cal benefit, reimbursement rate changes, HCBS, tracking Medi-Cal trends during PHE period and beyond.
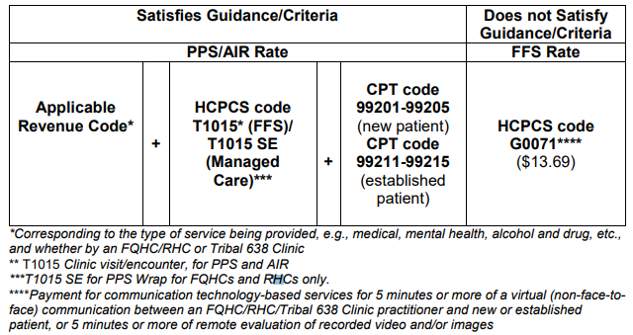
Below is a chart that outlines the associated HCPCS or CPT codes for billing either the Medi-Cal FFS rate or PPS rate.
Please Note:
DHCS is aware that FQHCs, RHCs, and Tribal 638 Clinics do not include CPT codes as part of traditional claim submission. That said, for purposes of the temporary flexibilities under this policy and to allow DHCS to track that services were provided via virtual/telephonic communication modalities, DHCS is requesting this modified billing structure relative to the Section III guidance, i.e., including the CPT codes on the “information line” of the claim form. The selected CPT codes will also allow DHCS to also track the level of complexity (low, medium, high, etc.) of the visit and whether it is a new or established patient.
Medi-Cal FFS:
For the PPS rate, FQHCs/RHCs would need to list HCPCS code T1015 in the “payable” claim line in conjunction with one of the appropriate corresponding CPT codes (i.e., 99201-99203 for “new” patients, and 99212-99214 for “established patients) on the “informational” line relative to the complexity of the virtual/telephonic communication. Please note that the corresponding CPT codes are not separately reimbursed, but instead will be used to identify the virtual/telephonic communication visit as well as by DHCS for tracking and reporting purposes related to COVID-19.
For the Medi-Cal FFS rate when billing with the HCPCS code G0071, clinics should only list the HCPCS code on the “payable” claim line and should not include a corresponding CPT code.
Medi-Cal Managed Care:
FQHCs/RHCs will receive their PPS rate, as applicable, for rendering a Medi-Cal covered benefits or services – whether provided through telehealth or virtual/telephonic communication – if they meet the criteria/guidance.
DHCS will ensure the FQHCs/RHCs are made whole with an appropriate wrap payment, consistent with existing DHCS policy.
FAQs
Medi-Cal Fee-For-Service
Informed Consent Requirements Prior to COVID-19
Health care providers must inform the patient about the use of telehealth and obtain verbal or written consent from the patient for the use of telehealth as an acceptable mode of delivering health care services.
If a health care provider, whether at the originating site or distant site, maintains a general consent agreement that specifically mentions use of telehealth as an acceptable modality for delivery of services, then this is sufficient for documentation of patient consent and should be kept in the patient’s medical file.
The consent shall be documented in the patient’s medical file upon DHCS request. Consent shall including the following:
- A description of the risks, benefits and consequences of telemedicine
- The patient retains the right to withdraw at any time
- All existing confidentiality protections apply
- The patient has access to all transmitted medical information
- No dissemination of any patient images or information to other entities without further written consent
Documentation
All health care practitioners providing covered benefits or services must maintain appropriate documentation to substantiate the corresponding technical and professional components of billed CPT or HCPCS codes.
Documentation for benefits or services delivered via telehealth should be the same as for a comparable in-person service.
Additional Resources
Providers may contant and email questions about Medi-Cal telehealth policy here.
California Department of Health Care Services Medi-Cal Program Telehealth Webpage
California Department of Health Care Services COVID-19 Resource Page
California Department of Managed Health Care COVID-19 Resource Page
CTRC has updated its Telehealth Reimbursement Guide effective Spring 2022. The guide includes telehealth reimbursement policies for Medicare, Medi-Cal Fee-For-Service, and some Managed Care plans. We have also expanded and updated the reimbursement information and scenarios specific to FQHCs and RHCs.